If there is one life or death issue for a Covered Entity and its Business Associate, it has to be HIPAA compliance. This is one point that could determine whether they will continue to be in business or fold up. This underlines the criticality of HIPAA compliance for a Covered Entity and a Business Associate.
While providing the appropriate patient rights and controls on its uses and disclosures is important to show compliance with HIPAA, a Covered Entity or a Business Associate needs to do more: it has to also to demonstrate this.
The CE or BA should also have performed the appropriate analysis of the risks to the confidentiality, integrity, and availability of electronic Protected Health Information (PHI). Unless this is done in a compliant manner, the CE or BA cannot ensure that it is protecting the PHI from vulnerabilities. Loss of a device holding data, accidental acts or intentional acts, such as cyberattacks, which have only become accentuated in recent times, are some of these.
Given the utter vitality of ensuring HIPAA compliance, shouldn’t Covered Entities and their Business Associates get a proper and thorough understanding of how to do this? This learning will be imparted at a webinar that is being organized on September 9 by MentorHealth, a leading provider of professional training for all the areas of healthcare.
The doyen of HIPAA compliance, Jim Sheldon Dean, will be the expert at this webinar, at which he will explain a 10-step method that will help participants gain thorough clarity of HIPAA compliance. Please register for this webinar by visiting https://www.mentorhealth.com/webinar/the-10-step-hipaa-compliance-review—how-to-ensure-your-compliance-is-up-to-date-801767LIVE?wordpress-SEO.
————————————————————————————————————–
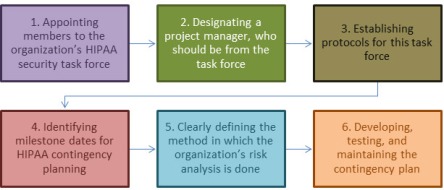
The expert will show how a Covered Entity or a Business Associate can ensure HIPAA compliance in a structured and logical manner over just ten days and thus escape enforcement actions from the HHS. He will explain how to carry these out in the 10-day span, which will be laid out in this manner:
- Day One: Research of Your Operations
- Day Two: Limitations on Uses and Disclosures
- Day Three: Patient Rights under HIPAA
- Day Four: HIPAA Risk Analysis
- Day Five: HIPAA Security Safeguards
- Day Six: HIPAA Security and Breach Notification Policies and Procedures
- Day Seven: Documentation of Policies and Procedures
- Day Eight: Training in Policies and Procedures Related to HIPAA
- Day Nine: Verification and Audits of Compliance
- Day Ten: Long Term Compliance Planning and Risk Management
The following areas will be covered at this webinar:
- Find out how to relate your office’s activities to the regulations
- Learn what are the ways you can share information under HIPAA, and the ways you may not
- Find out about HIPAA requirements for access and patient preferences, as well as the requirements to protect PHI
- Learn how to use an information security management process to evaluate risks and make decisions about how best to protect PHI and meet patient needs and desires
- Find out what policies and procedures you should have in place for dealing with e- mail and texting, as well as any new technology
- Learn about the training and education that must take place to ensure your staff uses e- mail and texting properly and does not risk exposure of PHI
- Find out the steps that must be followed in the event of a breach of PHI
- Learn about how the HIPAA audit and enforcement activities are now being increased and what you need to do to survive a HIPAA audit.
—————————————————————————————————————
About the expert: Jim Sheldon-Dean is the founder and director of compliance services at Lewis Creek Systems, LLC, a Vermont-based consulting firm founded in 1982, providing information privacy and security regulatory compliance services to a wide variety of health care entities.
Sheldon-Dean has more than 30 years of experience in policy analysis and implementation, business process analysis, information systems and software development. His experience includes leading the development of health care related Web sites; award-winning, best-selling commercial utility software; and mission-critical, fault-tolerant communications satellite control systems.





 This has led to confusion in many cases because rules that apply to certain kinds of electronic communication do not apply to others. Texting is a classic instance of this ambivalence. Since HIPAA has framed very broad guidelines to cover all electronic communication; some of its definitions of phrases are open to subjective interpretation.Resort to the Privacy and Security Rule
This has led to confusion in many cases because rules that apply to certain kinds of electronic communication do not apply to others. Texting is a classic instance of this ambivalence. Since HIPAA has framed very broad guidelines to cover all electronic communication; some of its definitions of phrases are open to subjective interpretation.Resort to the Privacy and Security Rule



























 Even though the risk is lower, it doesn’t remove all potential sources of risk. Any situation in which a third party can run code on a server has the potential to be exploited. If an attacker were able to brute force a user account on the server, they might be able to access private information that would typically be inaccessible to that account. It’s also possible that remote code execution vulnerabilities in other software could be exploited by an attacker to gain local access and run Spectre and Meltdown code.
Even though the risk is lower, it doesn’t remove all potential sources of risk. Any situation in which a third party can run code on a server has the potential to be exploited. If an attacker were able to brute force a user account on the server, they might be able to access private information that would typically be inaccessible to that account. It’s also possible that remote code execution vulnerabilities in other software could be exploited by an attacker to gain local access and run Spectre and Meltdown code.